Around this time of the year we get a lot of questions regarding flu vaccination. Typically though it’s really just one question, which is, “do you recommend I get the flu vaccine”? Any time there’s a question regarding vaccination, the answer is highly dependent on the individual asking and the particular vaccine in question. This is because not all individuals carry the same risk for acquiring a particular disease and not all vaccines have the same efficacy at preventing infection and/or preventing complications if there is infection. In order to answer the question of whether the flu vaccine is worth your while, we first need a little foundational education on the flu vaccine itself.
Vaccine Background
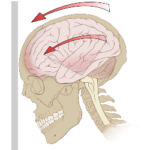
Flu vaccines, like all vaccines, are attempting to provoke a response by the immune system to produce antibodies. The antibodies produced will be specific to the particular antigens (antibody generator) present on the virus within the vaccine. The antibodies produced will circulate through the body looking for these particular antigens in order to produce a swift eradication before viral replication and illness can set in. These antibodies can circulate for months to years giving the individual immunity to the virus.
Antigenic Drift/Shift
Just like humans and animals, viruses are constantly evolving. Their genetic makeup is ever changing, which includes their antigens. The phenomenon of slow antigenic change is known as “antigenic drift”, where a more abrupt change is known as “antigenic shift”. This is problematic since flu vaccine production isn’t done using the current strain(s) of flu virus. Researchers at the CDC have to make their best guess using various forms of monitoring as to which flu virus is going to circulate in the upcoming year and hope that “antigenic drift” hasn’t made the antigens within the vaccine too different from this year’s virus. The more different the antigens are, the less effective the vaccine.
Those at Greater Risk
Symptoms of influenza are typically; fever, cough, sore throat, chills, fatigue, headache, runny nose, body aches, and occasionally vomiting and/or diarrhea. Influenza is typically self-limiting, resolving on its own within 1-2 weeks; however, it can progress into more serious conditions such as pneumonia and bronchitis. The most obvious individuals at greater risk would be those with suppressed immune systems; such as those with HIV/AID’s, cancer, children less than 2 years, or chronic steroid use. Other conditions such as those with renal failure, liver disease, or chronic lung disease create a greater risk of complications. The actual prevalence of influenza cases each year is much smaller than the CDC or any other health agency reports. There are many viruses, bacteria, and systemic illnesses that produce symptoms similar to influenza and so, are assumed to be, but they’re not. Reported cases of influenza are rarely confirmed, but rather presumptive diagnoses based on symptom picture.
Effectiveness?
So, let’s look at the research. The primary goal of vaccination is to prevent infection, prevent spread of infection, or at least decrease severity and/or complications of infection. Below, I’ve provided some research looking at these primary goals of flu vaccination.
In 2009 review by the Cochrane Collaboration evaluated the effects of vaccines against influenza in healthy adults. The researchers came to the following conclusion:
“There is not enough evidence to decide whether routine vaccination to prevent influenza in healthy adults is effective… The results of this review seem to discourage the utilization of vaccination against influenza in healthy adults as a routine public health measure1.”
In 2005 a study published in the Archives of Internal Medicine examined the influenza related deaths in the entire US elderly population. Despite increased widespread vaccination, which should produce a corresponding decrease in influenza related illnesses, however, what they found is stated below:
“…the 50-percentage-point increase in vaccination coverage among the elderly after 1980 should have reduced both excess P&I [Pneumonia and Influenza] and excess all-cause mortality by about 35% to 40%. We found no evidence to indicate that such a reduction had occurred in excess P&I or excess all-cause mortality in any elderly age group2.”
The CDC currently recommends children 6 months and older get a flu vaccine. A 2008 study found no evidence as to the benefits of flu vaccination in children under two years of age.
“…vaccine effectiveness was not clearly shown in children under 2 years of age. Further studies using different methods, in different locations, and in different seasons, are needed to clarify the effectiveness of influenza vaccine among young children3.”
In 2012 a comprehensive review of 75 randomized control studies in healthy children under 16 years of age was published. Researchers discuss their findings below:
“Inactivated vaccines in children aged two years or younger are not significantly more efficacious than placebo… little evidence is available for children younger than two years of age… In specific cases, influenza vaccines were associated with serious harms such as narcolepsy and febrile convulsions. It was surprising to find only one study of inactivated vaccine in children under two years, given current recommendations to vaccinate healthy children from six months of age in the USA, Canada, parts of Europe and Australia. If immunization in children is to be recommended as a public health policy, large-scale studies assessing important outcomes, and directly comparing vaccine types are urgently required4.”
The vaccine did not prevent emergency room visits or inpatient/outpatient visits during the years 2003-2005.
“Each year, US children aged 6 to 59 months experience high rates of hospitalizations, ED [Emergency Department] visits, and outpatient visits due to influenza. Despite this, we were unable, across 3 large communities to demonstrate that influenza vaccination was effective in preventing influenza-related inpatient/ED visits or outpatient visits during 2 consecutive seasons (2003-2004 and 2004-2005) among 6- to 23-month-olds, 24- to 59-month-olds, or the entire age span5.”
As a whole, reliable evidence of flu vaccinations efficacy is minimal. Most flu vaccine trials were funded by industry and those showing favorable efficacy were published in more prestigious journals. Those studies that were not funded by industry tended to find less favorable conclusions to flu vaccines. Former Chief Vaccine Officer at the FDA states: “there is no evidence that any influenza vaccine thus far developed is effective in preventing or mitigating any attack of influenza.”
The recommendation I make concerning the influenza vaccine is always an individualized one. I have to take the above factors into consideration, but in the end it’s about educating my patients so they are able to play an active role in their health care and make an informed decision for themselves.
Works Cited
- Demicheli V, Di Pietrantonj C, Jefferson T, Rivetti A, Rivetti D, “Vaccines for preventing influenza in healthy adults (Review),” The Cochrane Collaboration, 2009.
- Lone Simonsen, PhD; Thomas A. Reichert, MD, PhD; Cecile Viboud, PhD; William C. Blackwelder, PhD; Robert J. Taylor, PhD; Mark A. Miller, MD, “Impact of Influenza Vaccination on Seasonal Mortality in the US Elderly Population,” JAMA Internal Medicine, February 14, 2005, vol. 165, no. 3, http://archinte.jamanetwork.com/article.aspx?articleid=486407
- Megumi Fujieda, Akiko Maeda, Kyoko Kondo,Wakaba Fukushima, Satoko Ohfuji, Masaro Kaji, Yoshio Hirota, “Influenza vaccine effectiveness and confounding factors among young children,” Vaccine, 2008, pp. 6481-6485
- Jefferson T, Rivetti A, Di Pietrantonj C, Demicheli V, Ferroni E, “Vaccines for preventing influenza in healthy children (Review),” The Cochrane Library, 2012, Issue 8.
- Peter G. Szilagyi, MD, MPH; Gerry Fairbrother, PhD; Marie R. Griffin, MD, MPH; Richard W. Hornung, DrPH; Stephanie Donauer, MS; et al., “Influenza Vaccine Effectiveness Among Children 6 to 59 Months of Age During 2 Influenza Seasons,” Archives of Pediatric and Adolescent Medicine, October 2008, pp. 943-951.